47 yr old male presented to OPD with Pain Abdomen
47 M came with chief complaints
-Fever since 2 days
-vomiting since 2 days
-pain in abdomen since 2 days
-Burning micturition since 2 days
HOPI:
patient was apparently asymptomatic 2 days ago, then he developed fever which is ,intermitent, associated with chills and rigor,relieved on medication,
- vomiting from 2 days, food as content,non -projectile,3 episodes / day
-pain in abdomen from 2 days, pricking type,non radiating,in right hypochondrium
- burning micturition from 2 days
-uprolling of eyes,stiffness of both upper limbs yesterday
PAST HISTORY:
K/C/O epilepsy 15 years ago, 3 episodes
N/k/C/O Diabetes mellitus,asthma,tb
H/O fracture of left lower limb 15 years ago and operated
PRESENT HISTORY:
Appetite -Nornal
Diet-Mixed
Sleep-Adequate
Bladder habits-regular
Bowel habits-regular
Addiction:used to binge alcohol 15 years ago ,then after drinks occasionally
GENERAL EXAMINATION:
patient is conscious, coherent, co-operative,well oriented to time,place, person
No pallor,icterus,cyanosis, clubbing,pedal oedema - present,lymphadenopathy
Vitals:
PR:82bpm
BP:140/70mm Hg
Temperature:97F
RR:24cpm
SYSTEMIC EXAMINATION:
ABDOMINAL EXAMINATION:
Inspection:
Shape of abdomen:Scaphoid
Umbilicus:Central
All quadrants moving equally with respiration
No scars, sinuses,engorged veins
Palpation:
All inspectory findings are confirmed
No local rise of temperature,no tenderness
No gaurding , rigidity
No organomegaly
Percussion:
Reasonant note upto 5th ICS
No fluid thrill
Auscultation:
Bowel sounds heard
PROVISIONAL DIAGNOSIS:
INFLAMMATORY BOWEL DISEASE
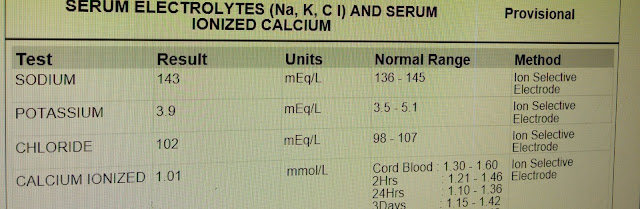
INVESTIGATIONS:
CBP:
15/10/22
16/10/22
Day1
1)NBM till further orders
2)IVF -NS,RL,DNS@50 ml/hr
3)INJ.MONOCEF 1 gm /IV/BD
4)INJ.METROGYL 500mg /IV/TID
5)INJ.PAN 40 mg IV/OD
6)INJ.ZOFER 4 mg IV/OD
7)INJ.TRAMADOL 1 AMP IN 100 ml NS/IV/BD
8)T.LEVIPIL 500mg PO/BD

















Comments
Post a Comment