1801006032 SHORT CASE
28 years old male presented to OPD
CHIEF COMPLAINTS:
1)Generalised weakness since 2 weeks
2)Shortness of breath since 2 weeks
3)Easy fatigability since 2 weeks
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 weeks back then he developed generalised weakness insidious in onset, gradually progressive
Shortness of breath of grade 2 which is insidious onset, which is grade 2 (NYHA classification) - slight limitation of activity -ordinary activity results in fatigue) ,no aggrevating and no relieving factors
Easy fatigability present
No c/o fever, nausea, vomiting, chest pain, pain abdomen, blood in stools, loose stools, sweating
PAST HISTORY:
Not a known case of DM/HTN/TB/Epilepsy/Thyroid abnormalities/Asthma
PERSONAL HISTORY:
Decreased appetite since 5-6 months
Takes vegetarian diet
Bowels and bladder habits are regular
sleep is regular
No addictions
FAMILY HISTORY:
No significant family history
TREATMENT HISTORY:
No significant history
GENERAL EXAMINATION:
Patient is conscious, coherent, cooperative
*Pallor is present
No signs of icterus,cyanosis, clubbing,
lymphadenopathy, pedal edema
Vitals:
Temp: afebrile
PR: 90 bpm
RR: 22 /min
BP: 140/80 mm hg
Systemic examination:
CVS: S1 S2 heard, No Murmur
RS: Bilateral air entry present
CNS: No focal neurological deficit
Per Abdomen : soft, non tender, no hepatosplenomegaly
Bowel sounds heard
INVESTIGATIONS:
Peripheral smear::
Serum creatinine:
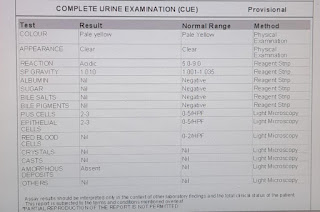
Complete Urine Examination::
Provisional Diagnosis:
Anemia secondary to vitamin B12 deficiency and iron deficiency (dimorphic anemia)
TREATMENT :
Inj. VITCOFOL 1000mg/IM/OD












Comments
Post a Comment