1801006032 LONG CASE
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
55years old female came to OPD with
chief complaints of
1) Fever since 14 days
2) Abdominal pain since 10 days,
3) shortness of breath since 10 days
4) vomitings since 3 days
History of present illness
Patient was apparently asymptomatic 14 days back then she developed Fever, which is insidious in onset, low grade , intermittent, associated with chills and rigor with no aggrevating factors and relieved on medication on first 2 days
then she developed Abdominal pain since 10 days,which is insidious in onset, gradually progressive, she localised the pain to her right upper quadrant, it was sharp in nature and not radiating ,no aggregating factors ,relieved temporarily on medication
then she developed shortness of breath, since 10 days,which is insidious onset, which is grade 2 (NYHA classification) - slight limitation of activity -ordinary activity results in fatigue) ,no aggrevating and no relieving factors and not associated with orthopnea and paroxysmal nocturnal dyspnea
She had history of vomitings prior to the day joining in the hospital which is of 2 episodes, watery in consistency ,non projectile,non bile stained,non foul smelling and non blood stained
Associated with generalized weakness and decreased urine output since from the day prior to the hospitalization
No history of trauma
Timeline of illness:
Patient was normal 14 days back then she developed fever for which she went RMP doctor, medication was given and symptoms got subsided
|
after 3 days she developed abdominal pain which is sudden and severe for which she went to hospital and diagnosed as AKI she given medication for 5 days and symptomatic relief present
|
then on 13/3/23 she developed generalized weakness, shortness of breath,abdominal pain,vomitings which led to hospitalization
Past history
She diagnosed with hypertension since 1year for which she taking medication (telma H)
No history of diabetes mellitus, tuberculosis, asthma, thyroid, epilepsy
No history of previous surgeries and no previous hospitalization
Family history:
No significant family history
Personal history:
Daily routine activities:
She usually wakeup at 6 AM, completes her regular activities in an hour
|
Around 8 AM she takes her breakfast (rice and vegetables curry) and goes to market as she sell lemons from past 20 years
|
and lunch at 1 PM and came to home at 5PM and takes a cup of tea and
|
she takes dinner at 9 PM
(She has an habit of taking alcohol around 10-20 ml,while going to bed) once in 3 days since 15 years)
Diet: mixed
Sleep: reduced since 10days
Bowel movement: regular
Bladder movement: reduced since 10days
Addiction: (She has an habit of taking alcohol around 10-20 ml,while going to bed) once in 3 days since 15 years)
General examination: patient is conscious, coherent, cooperative well oriented with time ,place, person
Moderately nourished and moderately built
Pallor: mild
Icterus: mild
Cyanosis: absent
Clubbing: absent
Lymphadenopathy: absent
Edema: absent
Vitals:
Pulse rate: 80bpm
Blood pressure: 140/80
Respiratory rate: 26 cycles per minute
Temperature:
Fever chart:
Systemic examination:
Abdominal examination:
INSPECTION:
Shape round (generalized distension)
Umbilicus - slightly retracted and inverted (normal)
Equal symmetrical movements in all the quadrants with respiration.
No visible pulsation, peristalsis, dilated veins and localized swellings.
PALPATION:
SUPERFICIAL : local rise of temperature and tenderness in right hypochondrium, epigastrium
DEEP : enlarged liver, extent upto 4cm below the costal margin,(confirmed by percussion)
Rounded edges soft in consistency, tender, moving with respiration non pulsatile,
No splenomegaly
Abdominal girth : 105cm
Xiphisterum to umbilicus:22cm (indicates umbilicus displaced downwards due to hepatosplenomegaly)
Umbilicus to pubic symphysis:14cm
PERCUSSION:
Hepatomegaly,liver span of 14cm with 4cm extended below the costal margin
Fluid thrill and shifting dullness absent
puddle sign absent
AUSCULTATION:
Bowel sounds are heard
RESPIRATORY SYSTEM:
Trachea central
Bilateral air entry
Normal vesicular breath sounds present
CENTRAL NERVOUS SYSTEM:
No focal neurological deficit
CARDIOVASCULAR SYSTEM:
S1,S2 sounds heard,no murmur are seen
DD:
Viral hepatitis?
Cholecystitis?
Alcoholic hepatitis?
Sepsis?
INVESTIGATIONS:
1) USG abdomen:
Findings- 5 mm calculus noted in gall bladder with GB sludge
Impression- Cholithiasis with GB sludge
Grade 2 fatty liver with hepatomegaly
2)Renal Function Tests:
13th
Blood urea 58
Serum creatinine 1.9
serum Na 127
Serum K 3.4
Serum Cl 92
14th
Blood urea 64
Serum creatinine 2.1
serum Na 117
Serum K 3.4
Serum Cl 70
15th
Blood urea 64
Serum creatinine 1.6
serum Na 125
Serum K 3.0
Serum Cl 88
3)LIVER FUNCTION TEST:
14th
Total bilirubin:2.6*
Direct bilirubin: 1.1*
Indirect bilirubin:1.5*
Alkaline phosphatase:193*
AST:37
ALT:21
Protein total: 7.0
Albumin:4.3
Globulin:2.7
Albumin and globulin ratio:1.6
4)Complete Urine Examination:
Albumin:+
Sugar: nil
pus cells:3-6
epithelial cells-2-4
urinary na 116
urinary k 8
urinary cl 128
5) Arterial blood gas:
Pco2: 23.3
PH: 7.525
Hco3: 23
Po2: 80.8
6) x ray Abdomen
7) complete blood picture:
13-3-23
Haemoglobin:11.7
Red blood cells:3.81
Pcv:32.5
Platelet count:5.0
Total leucocyte count:22,400
8)ECG:
9)lipid profile:
Total cholesterol:218mg/dl
Triglycerides:240mg/dl
HDL cholestrol:54 mg/dl
LDL cholestrol:116mg/dl
VLDL Cholestrol:48mg/dl
10)dengue
Ns1antigen test negative
11) thyroid function test:
T3:0.33
T4:10.46
Tsh:3.30
On 15/3/23/
Total leucocyte count:26,000
Serum calcium:0.92
PROVISIONAL DIAGNOSIS:
Non Alcoholic steatohepatitis
AKI secondary to sepsis(?)
Cholelithiasis
TREATMENT PLAN:
Liquid diet
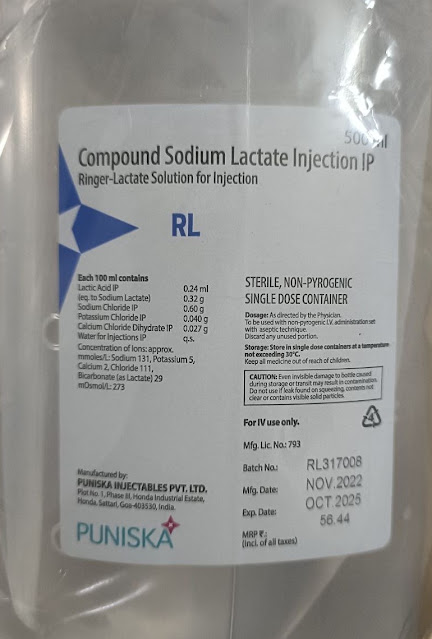
1. Iv fluids 1 unit NS, RL, DNS 100 ml/hr
2. Inj PAN 40 mg iv/ od
3. Inj PIPTAZ 2.25mg/iv/TID
4. Inj. METROGYL 500mg / iv/tid
5. Inj zofer 4mg iv/sos
6.INJ NEOMOL 1gm iv/sos
7.T.PCM 650mg po/tid
8.T.CINOD 10mg po/od

















Comments
Post a Comment